Mental Health



MOSAIC, Inc. Work Group Meeting 12/30/2010
“Integrative Collaborative Partnership with the Criminal Justice System & the Mental Health System"
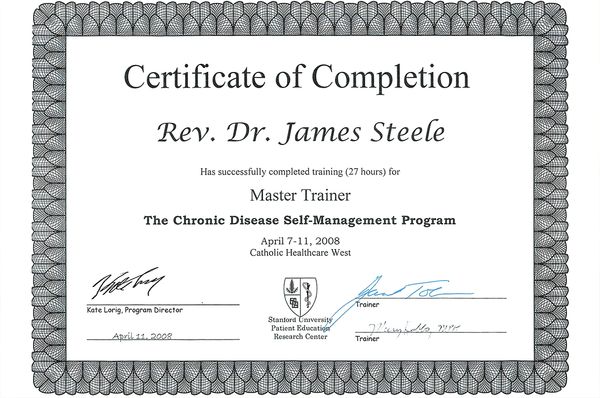
Honorable Judge Peter Espinosa & Rev. Dr. James Steele
MOSAIC Work-group Meeting, 12/30/10, by the Grace of God, through the Holy Spirit, Mysteries of Spiritual Awareness In Communities MOSAIC, Inc., Board of Directors, in an “Integrated Collaborative Partnership” with Honorable Judge Peter Espinoza, and Executive Administrator, Sandra Rodarte, THANKS TO ALL participants for their interactive dialogue, contribution and creative/innovative solutions to developing and establishing a logistical partnership strategy to eliminating future hierarchical bureaucratic barriers, in prisons & Mental Health!!!
- Honorable Judge Peter Espinoza, Supervising L.A. County Criminal Court Judge
- Hon. Judge Maria Stratton, Supervising L.A. County Mental Health Court Judge
- Deputy Mayor Guillermo Cespedes, City of Los Angeles
- Fabian Garcia, City of Los Angeles, Mayors Office
- Jose Ibarra-Virgen, City of Los Angeles, Mayors Office
- Councilman Juventino Gomez, City of El Monte
- Alex Johnson, L.A. County, Supervisor Mark Ridley-Thomas
- Richard P. Fajardo, L.A.C. Sr Deputy for Justice, Supervisor Mark Ridley-Thomas
- Dr. Kathleen Daly, DMH Director of Jails
- James Preis, Executive Director, Mental Health Advocacy Services
- D. Sheila Price, California State University Los Angeles Professor
- Wilfred Paltanwala, DMH Adult System of Care Administrator
- Neena Paltanwala, DMH Training
- Rabbi Israel Hirsch, LAPD Chaplain
- Rev. Eddie Parsadanian, Church of the Living Word of God Pastor
- Rev. Dr. James N. Schultz, Atwater Park Baptist Church Pastor
- Rev. J. Deron Johnson, Pasadena CME Church Pastor
- Rev. Dr. James Wm. Steele, MOSAIC, Inc., CEO
God’s Blessings Always and Forever & Ever!!!
Focus of meeting: A MOSAIC Journey “a new heart….a new spirit” (Eze 36:26). A Positive perspective to working together, is taken from the words of Henri Nouwen’s, which our perspective today is: “Ministry is NOT only a communal experience, it is a mutual experience….The mystery of ministry is that we have been chosen to make our own limited & very conditional love the gateway for the unlimited and unconditional love of God. Therefore, true ministry must be mutual” (pp. 42,44).
As we move forward in this partnering movement and journey, “deinstitutionalization,” whether it be prison releases, long-term psychiatric care (mental illness issues) or independent-living arrangements within the community-at-large, all of these issues has forced us to acknowledge a growing awareness of the “fragmented service systems” we are struggling with each and every day. Therefore, together we can make a major difference by means of collaboratively partnering, secularly intertwined with World Faith Groups (WFGs) and/or Faith-based community organizations (yet remaining legally independent social service identities). For instance, “In United States….clergy outnumber psychiatrists by nearly ten to one and are much more equitably distributed geographically than any other Mental Health professional. A consistent finding over the past two decades indicates that approximately 40 % of persons seeking outside help with emotional distress turn first to the clergy, a figure considerably higher than for the next largest group” (Aist, 1987, p.299). Now, putting this into today’s pluralistic society perspective, if a person with mental illness or the family is not made to feel that he or she can find support and comfort with the congregation, then a vital support system is denied, which similarly apparent in our secular “fragmented social services systems.” The paramount ethical issue facing those dealing with mental illness today is not the propriety of the medication or whether a patient can refuse treatment or not. These are important, but they pale in comparison within the stigma attached to mental illness. The challenge for WFGs, Faith communities is to break down both hierarchical bureaucratic barriers, as well as the walls of ignorance and stigma so that understanding and support is forthcoming.
World Faith Groups (WFGs), Faith communities can be the place where people with mental illness, or lifestyle problems in general, find openness and hospitality as they participate in the life of the congregation and the community-at-large. Faith Groups, Faith communities can be a place that accepts and supports both the person who is ill and the family, caregivers as they face the realities of mental illness. Faith Groups, Faith communities can be a place where the person who has the illness is valued for who they are and for how he or she participates. This atmosphere can enable the person to feel a sense of increased self-worth, spiritual growth and empowerment.
The importance of the diverse resources of the WFGs, Faith communities in providing a response to people with mental illnesses cannot be overestimated. Jay Centifanti (1987), one of the founders of a national mental health consumer organization, said, “The beginning of my journey back was when people stopped treating me like I was disabled & incompetent & started treating me as though I was welcome at the table..” Therefore, MOSAIC Journey begins, here & NOW!!!
Books/Binders: These binders are full of very useful, practical, and resourceful material to guide and support our endeavors here today, but more importantly for the future. For instance,
SECTION 1: Work Group Meeting, 12/30/2010, AGENDA.
SECTION 2: is a Narrative Synopsis of MOSAIC, Inc., which describes our past, present, and planned activities: “Past” is our foundation, MISSION & VISION – “Present” is our GOALS:
How can this be done by MOSAIC, Inc.???
First: by starting with a TRAINING MANUAL!!! Which educates, trains and teaches advocacy methods and management to World Faith Groups (WFGs) and Faith-based Community Outreach to Mentally Ill by means of: WFGs: Who are they??? What relevancy does WFGs have on any specific community (e.g., Mentally Ill), as well as, the community-at-large and/or whole community!!!
What DMH “WFGs” strategic outreach plan has been created??? Established? Sustained??? and/or Self-Supporting and Self-Sustaining???
Faith Groups: Understanding them by means of a Comprehensive Comparative Outline: “Three Faith Groups”: (a) Judaism; (b) Islamic Sufism; (c) Christianity, re: (i) Motifs of Thought, (ii) Polity, (iii) Beliefs, (iv) Alternative Designations, (v) History, (vi) Sacred/Authoritative Sources, (vii) Ethics/ Practices, (viii) Divisions, (ix) Prominent Thinkers, (x) Membership, (xi) Worship, and (xii) Evaluations.
Faith Groups & Faith-based Community Organizations Infrastructure.
Outline that integrates Faith Groups & DMH (re: MHSA).
DMH & Faith-based Community Org. MOU’s / Partnership by means of: Master Business Plan: 1). Mission Statement, 2). Vision, 3). Situation Analysis, 4). Critical Assumptions, 5). Goals, 6). Objectives, 7). Strategies, 8). Action Plans, 9) Business Plan Valuation, 10). Monitoring/Evaluations.
MOSAIC Journey: A World Faith Groups (WFGs) Manual on Outreach Ministry and Mental Illness; Offenders: Challenge for State & Church Synopsis (Doctoral Thesis); WFGs Mentoring Ministries; “Family, Parent and/or Guardian Coaching” Program; “Family Focused Mentoring” Program, Family Preservation & Mentor Mom Program
How can the WFGs and Faith-based Community Organizations respond?
Second: “MOSAIC, Inc’s Faith Group Symposiums: Application and Implementation of Mental Illness Outreach Ministries and Spiritual Awareness” is an innovative collaboration to help & assist All WFGs have a better understanding of disabilities and/or mental illness & what we can do to be understanding & supportive of those who have disabilities and/or mental illness. The values of World Faith Groups living/lifestyles create the potential for creating caring congregation’s, mosque’s, etc.
In response to the needs of people with a disability and/or mental illness and their families/guardians, “Mysteries Of Spiritual Awareness In Communities MOSAIC, Inc.,” was created to facilitate the work, initiative, and collaboration of All of the World Faith Groups (WFGs) and Faith-based Community Organizations in reaching out to those who have a disability and/or mental illness and their families/guardians. The goal is to have them welcomed (into congregation’s, synagogue’s, etc.) as part of their Faith community and integrated into the life and lifestyle of that community.
“Mysteries Of Spiritual Awareness In Communities MOSAIC, Inc.,” appreciates that numerous WFGs/Communities have an educational system in place at the national, state, regional, local and congregation, synagogue, mosque and temple levels. This system can encourage and enable reaching out to people who have a disability, mental illness and to families/guardians by drawing them into the life and lifestyle of the particular Faith Group’s membership.
TOPICS: that are relevant to assisting community and secular organizations, government agencies, re:
# 1. What type of transition and/or strategies can support successful entry into the Mental Health System that involve initial & ongoing engagement & welcoming?
# 2. Once engaged into initial transition/services, identify & develop strategies that promote continued client engagement & motivation to move forward successive goals (e.g., recovery)?
# 3. How are we going to create community support systems for clients, families and/or caregivers who have moved thru the MH System & no longer require routine services from Mental Health Professionals?
NOTE: These three topics were suggestions by DMH to pursue, therefore, our participant Faith Groups Symposium recommendations are very relevant to supporting, assisting & partnering with DMH’s System.
SECTION 3: Mental Health Community Chaplaincy (MHCC): World Faith Groups (WFGs) pastoral counseling, including shamanism, ritual dances, & exorcism have made tremendous efforts to deal with mental illness & have been in the domain of religious practice thru-out history, & many believers turn first to clergy or a faith-based agency.
Churches, synagogues, temples and mosques serve as surrogate (extended) families, whereas, religious writings and spiritual practices bring solace, support, sharing, practical wisdom, etc.
People with incipient mental illness trust religious organizations far more than community health services.
Issue of separation of church & state, half of the LA agencies were reluctant to collaborate with government agencies, thereby, impeding access to treatment.
A case could be made for faith-based agencies' having consultative arrangements with mental health facilities, rather than faith-based organizations attempting to provide full-scale care.
Religious leaders and mental health professionals may differ markedly about basic concepts of psychological health and mental illness, which can yield to mutual respect, case-based consultation, education, & exchange of ideas between clergy & mental health professionals, Collaboration/consultation between clergy/mental health prof. can benefit persons with mental disorders.
All World Faith Groups and Belief Systems, need to foster communication & trust, re: Muslim religious leaders & mental health professionals to improve access to religiously/culturally appropriate psychiatric services. Imams are less likely than other clergy to have formal comprehensive counseling training.
The agencies of QueensCare Health and Faith Partnership, make-up a network of faith-based organizations, and parish nurses who provided health care in a low-income, ethnically diverse area of Los Angeles. Barriers to providing mental health services included limited professional training, reluctance to partner with government programs, and financial and staffing limitations.
Faith-based providers are the only source of care for some persons with mental disorders. However, little is known about the capacity and willingness of faith-based organizations to provide mental health services or the compatibility of these services with the organizations' religious values. Implementing mental health services within religious organizations could benefit some high-risk populations, such as recent immigrants, because they have limited access to medical services but high rates of participation in religious organizations. Religious organizations possess tangible resources, such as meeting space and staff members, as well as intangible resources, such as values of hope, healing, and community. Some faith-based communities also have health screening & education programs that could be extended to include mental health services.
Most representatives of Faith communities were interested in providing mental health services, suggesting that they would partner with most agencies, although half were reluctant to partner with government services. Partnering with other stakeholders may be one way to address barriers to implementing programs. For example, collaboration may facilitate access to evidence-based programs for low-income / minority populations, and faith-based mental health care may provide one avenue for bringing needed mental health services to low-income, ethnically diverse communities.
Persons with mental disorders seek initial treatment from clergy more frequently than from psychiatrists or general medical doctors, and a majority who seek treatment from clergy do so to the exclusion of other providers. However, little is known about the relationship between religion and use of the mental health care system.
Some have expressed concern that reliance on clergy may prevent or delay the appropriate use of mental health care, but the data collected does not support this notion.
Religiousness has a favorable impact on the quality of life of older adults with schizophrenia, and must be considered along with other therapeutically important agents.
Religion can help instill a positive sense of self, decrease the impact of symptoms, provide social contacts and religious issues need to be discussed in clinical settings.
Practitioners need to develop programs or services that are congruent with religious/spiritual beliefs & practices in order to better enhance the psychosocial well-being and improve the quality of life among older persons in rural areas. Therefore, spirituality/religiousness have been shown to be highly prevalent among patients with schizophrenia. However, clinicians are rarely aware of the importance of religion and understand little of the value or difficulties it presents to treatment.
Spirituality should be integrated into the psychosocial dimension of care. Little is known of the relations between psychosis, religion, suicide.
Persons with mental illnesses who are from ethnic minority groups are underserved, especially those with serious mental illness who represent above-average rates of homelessness, emergency visits, hospitalizations, and legal involvement, resulting in high risks of morbidity and relapse.
SAMHSA vision of "a life in the community for everyone," as their preferred future would be: Recovery is the expected outcome; Service recipients direct their own care; Evidence-based Services; & Performance management drives quality improvement. In next few years, every service:
1), CMHS will seriously consider embracing the concept and practice a public health model of health care.
2), We will use the tools of public health to advance holistic, person-centered health care.
3), The spirit of public health, which considers both the health of individuals and health of the community, we must attend to broad determinants of health.
4), The public health approach demands that prevention, early intervention, and treatment services be delivered by a customer-focused workforce. Practicing in a 21st century health care environment demands a competent, capable, sustainable, and culturally diverse workforce.
5), Health Care that is inclusive of individual, community, and social factors must demonstrate its value as measured by both short- and long-term outcomes—focusing on continuous quality improvement.
SECTION 6: National Alliance on Mental Illness (NAMI) issued a report card on the Public Mental Health System for adults, giving the nation a grade of D, re:. the system is "in shambles" in 2003. NAMI executive director Michael J. Fitzpatrick goes on to state: "Mental health care in America is in crisis."
Grading the States 2009 consists of report cards for each state, e.g., five states—Arizona, Calif., Connecticut, Hawaii, and Mass.—have "exemplary cultural competence plans and activities." California requires all county programs to identify groups facing significant disparities, develop comprehensive cultural competence plans, & report annually on progress. www.nami.org/grades09.
The Substance Abuse & Mental Health Services Administration (SAMHSA) has released the first update in its series of evidence-based practices toolkits. Assertive Com. Treatment Knowledge Informing Transformation (ACT KIT) is designed to help agencies implement, sustain, evaluate ACT programs & ensure that people with serious mental illness have access to these effective services, re:
1) Building Your Program, is designed to help mental health authorities, agency administrators, and ACT leaders think thru & dev. the structure of ACT programs. 2) Training Frontline Staff, is a workbook used as a training manual for group sessions & basic desk reference, divided training into four modules: 1. basic elements of ACT, 2. recovery and the stress-vulnerability model, 3. core processes of ACT, and 4. the array of services that ACT programs provide, from medication support to health promotion to housing assistance and employment. Both volumes focus particularly on the differences between assertive and coercive treatment and how to ensure that consumers' rights are respected.
3) Evaluating Your Program, shows quality assurance team members how to assess the effectiveness of the ACT program and includes a readiness assessment.
Finally, The Evidence, booklet introduces all stakeholders to the research literature.
The ACT KIT is available on Web site of the Center for Mental Health Services at mentalhealth.samhsa.gov/cmhs/communitysupport/toolkits.
Provider Attitudes Toward Evidence-Based Practices: have implications for dissemination of evidence-based practices & policy change. Contextual adaptations in evidence-based practice design & training may result in wider adoption of innovative and efficacious treatment practices.
“The Family Intervention Guide to Mental Illness: Recognizing Symptoms and Getting Treatment” book is a guide, for family members, for intervening in a loved one's mental illness. Step by step it walks through recognizing the illness, obtaining an evaluation, initiating treatment, & maintaining wellness.
From the beginning it champions family involvement as a key to recovery.
Treatment of Bipolar Illness book takes on the challenge of focusing on treatment providers, be they physicians or clinicians, and patients & their families. Topics cover bipolar treatment considerations: antidepressants, mood stabilizers, complex combination treatment, and childhood bipolar disorder.
SECTION 7: Homeless persons with mental illness mostly report the same reasons for loss of housing and continued homelessness as those who do not have a mental illness, thereby, reducing the risk of homelessness among persons with mental illness, as among other vulnerable social groups.
Collaborative care interventions that include psychotherapy can increase the likelihood that Latino patients receive preferred care.
The book “All God's Children: Inside the Dark and Violent World of Street Families,” is about the lives of young men & women grappling with long histories of abuse, pathology and vulnerability. Denfeld’s prologue states: street families are a "criminal subculture" that has gone unchecked. The work is thought provoking, sparking a debate on homeless youths and their survival on the streets.
Reaching Out and Engaging to Achieve Consumer Health (REACH), participation was associated with substantial increases in outpatient services as well as cost offsets in inpatient /emergency services & criminal justice system services. REACH was established in 2000 in response to concerns that homeless people with serious mental illness were being displaced by a new sports stadium, receiving from the state a $10.3 million competitive grant to implement integrated services for homeless clients with serious mental illness, adopting a housing-first program with a "whatever it takes" approach. This is to engage & house clients by providing assertive outreach through a homeless outreach team, multiple housing options, assertive com. treatment team-based case mgmt. and outpatient services.
These programs served as the model for the full-service partnerships, which became the cornerstone of the largest mental health policy intervention in recent times, California's MHSA.
The REACH program reduced the likelihood that clients would decompensate and be admitted to an inpatient or emergency facility or receive services in jails.
Risk Factors for Homelessness indicated that adversity in childhood & the risk of homelessness, point to the importance of early intervention efforts, e.g., separation of children from their parents or caregivers, including socioeconomic disadvantage, mental illness, and problems with drugs.
Today, in our pluralistic society, the public mental health system remains fragmented and complex. Therefore, we need to be creative and truly “innovative,” and I mean “innovate in the true sense of the word.” Then consider the concept, “building medical homes,” which provides key service elements shown to enhance access, care coordination, & quality of care. Although there will be great challenges to introducing mental health homes, and the rewards will be that individuals with serious mental illness will experience better physical health, mental health, and quality of life and that unnecessary social costs will be reduced.
The "medical home" concept was developed in primary care to provide accessible & accountable services for individuals with chronic medical conditions.
However, the public mental health system, as a means of managing its most intensive & comprehensive (and expensive, short of hospitalization) care, usually does not allow access to these services until individuals fail routine community care and experience treatment lapses, multiple hospitalizations, or involvement with criminal justice programs. The good news is that individuals are able to be supported in a meaningful/sustained recovery. On the other hand, individuals fall through the cracks of a fragmented system where accountability is not clearly and responsibly owned. This group typically includes those with severe and persistent mental illness, often with co-occurring substance abuse, who experience difficulty engaging and remaining in treatment. These individuals live on the fringes of our communities and their families and can be thought of as "homeless" from a system-of-care perspective, falling through gaps in care. Strategies for better engaging these individuals will require MH practitioners to expand their commitment to medical home principles.
Family and community outreach The mental health home extends current notions of family and support system outreach by engaging communities and families beyond individual treatment plans. The mental health home model adopts a "customer is always right," consumer-friendly ethos.
Useful guidelines in the systemic development and dissemination of a MH home approach are:
1). Communicating key concepts to stakeholders; 2). Training clinical staff in the MH home model; 3). Piloting initiatives with innovative providers; and 4). Exploring and testing reimbursement strategies.
A “New Justice Center Guide on Expanding Housing Options After Release From Incarceration” is so critically important today, because each year more than 735,000 people are released from prisons & an estimated nine million are released from jails (noting the fact that approximately 40,000 inmates from California prisons/jails are to be released into the community in the very near future).
The Council of State Governments Justice Center has a new publication—Reentry Housing Options: The Policymakers' Guide—that describes six alternatives for reentry housing, including their benefits and limitations. The options are private-market rental housing, public housing, affordable housing (nonprofit or privately owned & managed), halfway houses, supportive housing, and specialized reentry housing. The guide examines three approaches to enhance the availability of these housing options: 1) greater access, 2) increased housing stock, and 3) revitalized neighborhoods. The guide also provides case examples of how each approach has been put into action by a particular jurisdiction.
The authors of the guide note that no single housing approach will be a perfect fit for a jurisdiction. The guide is designed to help community leaders and policy makers increase their knowledge of reentry housing alternatives and specific approaches to creating more housing options to improve the chances that individuals will reenter the community safely and successfully.
Publication of “Reentry Housing Options: The Policymakers' Guide” was supported by the Bureau of Justice Assistance, U.S. Department of Justice, and is available at justicecenter.csg.org.
SECTION 8: “Conclusion” includes an overview of each of the Sections, “Pilot Project” Solutions, along with an overview of World Faith Groups strengths for members with Mental illnesses, as well as Strengths a Mental Health Agency brings to WFGs. Concluding with the statement by Henri Nouwen: “What we see, and like to see, is cure and change. But what we do not see and do not want to see is care, the participation in the pain, the solidarity in suffering, the sharing in the experience of brokenness.” So let’s share & partner together.
From a WFGs perspective, congregants rely on their pastor as a trusted advisor. They seek help with such practical issues as what to do when a crisis occurs, or a referral to a mental health professional who will respect their faith connection, or assistance in finding a living arrangement for their family member (e.g., getting released from jail, mental illness facility, etc.). The pastor can be a key person in assisting the person who is ill and/or the family by giving them information about community resources. He/she can act as a referral agent and a catalyst who can use the skills and energies of others, both members of the congregation and community professionals. In this way the pastor not only carries on the religious tradition of spiritual support, he/she also acts as a gatekeeper to open doors to additional resources (i.e., collaborating & partnering).
The WFGs pastor, rabbi, sheik, imam, priest, and clergy in the role of gatekeeper, has at least 3 tasks:
- Learning the scope and quality of public and private resources that serve people with mental illnesses and their families and ways to access these resources;
- Identify others who can help and empower them to do so. There are people within most congregations and professionals and organizations within the community who can provide valuable info & support to the person who is ill & the family; and
- Inspire confidence in the person who needs assistance and his/her family that these resources can be helpful.
In other words, a pastor/clergy facilitates to “Building Bridges” with Mental Health Systems, Providers, Organizations and community partners “……from the moment psychiatry emerged as a distinct profession, psychiatry and religion have overlapped and at times overtly competed. The reason for this is clear: both seek to heal forms of brokenness that stand on the ambiguous borderline between body and what is variously referred to as “psyche” or “spirit.” Psychiatry in its more biological phases often enjoys positive relations with religion; a division of labor can emerge in which psychiatry deals with mental illness that is primarily biological in origin, while religion deals mainly with moral and spiritual problems in living. On the other hand, there are totally positivistic forms of biological psychiatry that tend to reduce all human problems to their biological psychiatry foundations, thereby appearing to reject the relevance of religion in solving human problems” (Browning, 1990, p.4).
Faith Groups and mental health communities share a commitment to the emotional and spiritual well-tbeing of people whom they serve. Both see themselves as agents of healing. Both share the goal of promoting care. Both worlds share the goal of being compassionate toward those they serve. Both focus on promoting self-esteem and nurturing of the human spirit. Both work to create an atmosphere of receptivity and acceptance. Both encourage and support people in building relationships, and developing or recovering social patterns, vocational and recreational skills. Both work with people to help them overcome feelings of despair and powerlessness. Both encourage people to live with present possibilities, but to also recognize the hope of the future. Both agree that people who have a mental illness improve when they are able to participate in community settings, such as a congregation.
Cong. Strengths for Members with MI
- A commitment to be open & caring
- The ability to support members
- Com. knowledge & invest in well-being
- A link with the community
- Ability to affirm/encourage people’s talents
Cong. Strengths a MH Agency Brings
- Expertise about mental illness
- Asst. to clergy in pastoral ministry
- Providing prof. asst. caring for people
- Asst. addressing a community need
- Asst. & expertise developing prog.
MOSAIC, Inc., can most definitely bridge a much needed gap that exists in the Mental Health, Homelessness and Judicial Systems (i.e., Fragmented Systems). For instance, MOSAIC, Inc., takes a practical approach to outreach ministry and a multi-cultural, multi-educational perspective, which is to assist the mentally ill, homeless, offenders and ex-offenders holistically. In order to do this, chaplains, clergy and congregants must be willing to administer and coordinate what Maslow terms, the basic needs of survival, such as food and shelter. Then we get into the all-important, all-encompassing employment issue so vital for independence, so that one can provide for themselves, and feel good about doing so (self-esteem). MOSAIC, Inc., can remind each and every one of us at this “Work-group Meeting” as Judicial Court & Governmental Officials, Mental Health Professionals, Professors, Executive Directors, Chaplains, Pastors, or clergy, regardless how we perceive mental health or prison ministry, or the validity of inmate responses to Faith, the church serves as a continuing source of grace and hope for those who truly desire to change their lives.
Fr. Henri J.M. Nouwen, a Roman Catholic priest, shared the last seven years of his life with people with mental illnesses, as pastor of the I’Arche Daybreak community in Toronto, Canada, and he sums up MOSAIC, Inc.’s MOTTO: “…a new heart…a new spirit” (Eze. 36:26), as well as MISSION & VISION quite nicely in reference to Christ’s loving, sharing and caring ways to all peoples. Yet at times we all seem to “forget that Jesus did not give food to the many without having received some loaves and fishes from a stranger in the crowd: that He did not return the boy of Naim to his widowed mother without having felt her sorrow; that He did not raise Lazarus from the grave without tears and a sigh of distress that came straight from the heart. What we see, and like to see, is cure and change. But what we do not see and do not want to see is care, the participation in the pain, the solidarity in suffering, the sharing in the experience of brokenness” (1998: 31-32). So let’s share & partner together. AMEN!!!





Voice Awards honor positive portrayals of mental disorders
October 2005, Vol 36, No. 9
Russ Newman, PhD, JD, APA's executive director for professional practice, presented two awards at the 2005 Voice Awards, held in July in Los Angeles to acknowledge film, television and radio writers and producers who create what organizers call "dignified, respectful and accurate portrayals of people with mental health problems."
One of the awards Newman presented went to Sandy Climan, producer of the movie "The Aviator," for its positive portrayal of Howard Hughes's perseverance while facing phobias and obsessive-compulsive disorder. Newman also bestowed an award on Reverge Anselmo, writer and director of the movie "Stateside" for his portrayal of a schizophrenic woman in a relationship with a nonschizophrenic man.
"Our polls show that the public credits the media with helping to reduce the stigma around mental health issues," Newman says. "It's important to recognize the media who have contributed to that reduction."
Also honored, among others, were:
- Neal Baer, executive producer of "Law & Order: SVU" and former executive producer of "ER," for his work bringing mental health issues into the mainstream media through characters such as ER's Maggie Lockhart (played by Sally Field), who faced and ultimately overcame bipolar disorder.
- Brooke Shields, for her memoir, "Down Came the Rain: My Journey Through Postpartum Depression" (Hyperion, 2005).
- Maurice Bernard, who has bipolar disorder, for his portrayal of Sonny Corinthos on "General Hospital."
- The Spanish language network Univision, for its extensive coverage of mental health awareness through its program "Salud es Vida... ¡Entérate!" (Health is Life...Inform Yourself!).
- The respective producers of "Monk," "Huff" and "Scrubs," for their positive portrayal of people with mental health problems.
The Substance Abuse and Mental Health Services Administration (SAMHSA) created the Voice Awards as part of its Elimination of Barriers Initiative--a three-year pilot program launched in September 2003 to use public education to counter stigma and discrimination associated with mental illnesses. SAMHSA launched the program in collaboration with state mental health authorities in California, Florida, Massachusetts, North Carolina, Ohio, Pennsylvania, Texas and Wisconsin. Partners include APA, the American Psychiatric Foundation, the National Association of State Mental Health Program Directors and the Mental Health Media Partnership.
Attending the awards ceremony with Newman was Helen Mitternight, assistant executive director of public relations in APA's Practice Directorate.
"The Voice Awards were created to reduce the stigma of mental illness," says Mitternight, "which fits right in with part of APA's mission. By recognizing these people, we hope to encourage them to continue this kind of message in entertainment."
E. PACKARD
Copyright © 2022 A MOSAIC Journey - All Rights Reserved.